If there are elevated liver enzymes in your bloodstream, it indicates some abnormal condition. This elevation could be a temporary occurrence or a potential indicator of a medical condition such as hepatitis or liver disease. Additionally, certain medications have the potential to cause an increase in liver enzyme levels.
Table of Contents
ICD 10 code for elevated liver enzymes
ICD-10 code R74. 01 for Elevation of levels of liver transaminase levels is a medical classification as listed by WHO under the range – Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
Code R74.0 Nonspecific elevation of levels of transaminase and lactic acid dehydrogenase [LDH], has been expanded to separately report elevation of levels of liver transaminase (R74.01) and elevation of levels of LDH (R74.02). Code R74.01 includes elevation of levels of alanine transaminase (ALT) and aspartate transaminase (AST).It’s important to distinguish elevations of different liver enzymes because they can result in different clinical treatment modalities and resource utilization.
Liver enzymes and normal values
Liver enzymes play a crucial role as proteins that facilitate the acceleration of chemical reactions within your body. These essential reactions encompass the production of bile and substances aiding blood clotting, the breakdown of food and toxins, and the immune system’s fight against infections. Prominent liver enzymes include:
⦁ Alkaline phosphatase (ALP). normal: 44-147 U/L
⦁ Alanine transaminase (ALT). normal: 29-33(males), 19-25(females)
⦁ Aspartate transaminase (AST). normal: 14-20(males), 10-36(females)
⦁ Gamma-glutamyl transferase (GGT). normal: 0 to 30 IU/L
When your liver sustains damage, it releases enzymes into your bloodstream, with ALT or AST being the most frequently detected enzymes in this context.
Tests for liver enzymes
A set of specialized blood tests is frequently employed to determine the liver’s status, whether it is inflamed, injured, or functioning properly. These tests can also differentiate between acute and chronic liver disorders, as well as discern between hepatitis (liver infection or inflammation) and cholestasis (disruption in bile formation or obstruction in bile flow).
The commonly conducted blood tests encompass:
Functional Tests:
- Serum Bilirubin Test: This gauges bilirubin levels in the blood, a product of the liver excreted in bile. Elevated bilirubin levels may indicate bile flow obstruction or issues in bile processing by the liver.
- Serum Albumin Test: This assesses albumin levels, a blood protein useful in diagnosing liver disease. Low albumin levels may suggest impaired liver function.
- International Normalized Ratio (INR), formerly Prothrombin Time (PT) Test: This measures blood clotting time, dependent on vitamin K and a liver-produced protein. Prolonged clotting may indicate liver disease or deficiencies in specific clotting factors.
Liver Enzymes: - Serum Alkaline Phosphatase Test: Measures alkaline phosphatase levels, an enzyme found in various tissues, with high concentrations in the liver, biliary tract, and bone. It assesses liver function and identifies lesions causing biliary obstruction.
- Alanine Transaminase (ALT) Test: Measures alanine aminotransferase levels, an enzyme mainly found in the liver. Elevated levels indicate acute liver cell damage, aiding in liver function assessment and treatment evaluation for conditions like hepatitis.
- Aspartate Transaminase (AST) Test: Measures aspartate transaminase levels, an enzyme found in multiple organs. Elevated levels signal liver or heart problems and are indicative of acute liver cell damage.
- Gamma-Glutamyl Transpeptidase Test: Measures gamma-glutamyl transpeptidase levels, an enzyme produced in the liver, pancreas, and biliary tract. This test evaluates liver function, provides information on liver diseases, and detects alcohol ingestion.
- Lactic Dehydrogenase Test: Detects tissue damage and aids in liver disease diagnosis, although it is nonspecific and rarely used for liver assessments.
- 5′-Nucleotidase Test: Measures 5′-nucleotidase levels, an enzyme specific to the liver. Elevated levels are associated with liver diseases, especially those linked to cholestasis.
Additional Diagnostic Tests: - Alpha-Fetoprotein Test: Evaluates alpha-fetoprotein levels, a blood protein made by fetal tissue and tumors. It predicts the risk of primary liver cancer and monitors therapy effectiveness in certain cancers.
- Mitochondrial Antibodies Test: Detects the presence of antibodies indicating primary biliary cirrhosis, chronic active hepatitis, and other autoimmune disorders.
- Serum Alpha-1 Antitrypsin Test (A1AT): Measures alpha-1 antitrypsin levels, aiding in identifying a rare form of emphysema in adults and a rare form of liver disease (cirrhosis) in children and adults.
What do elevated liver enzymes indicate?
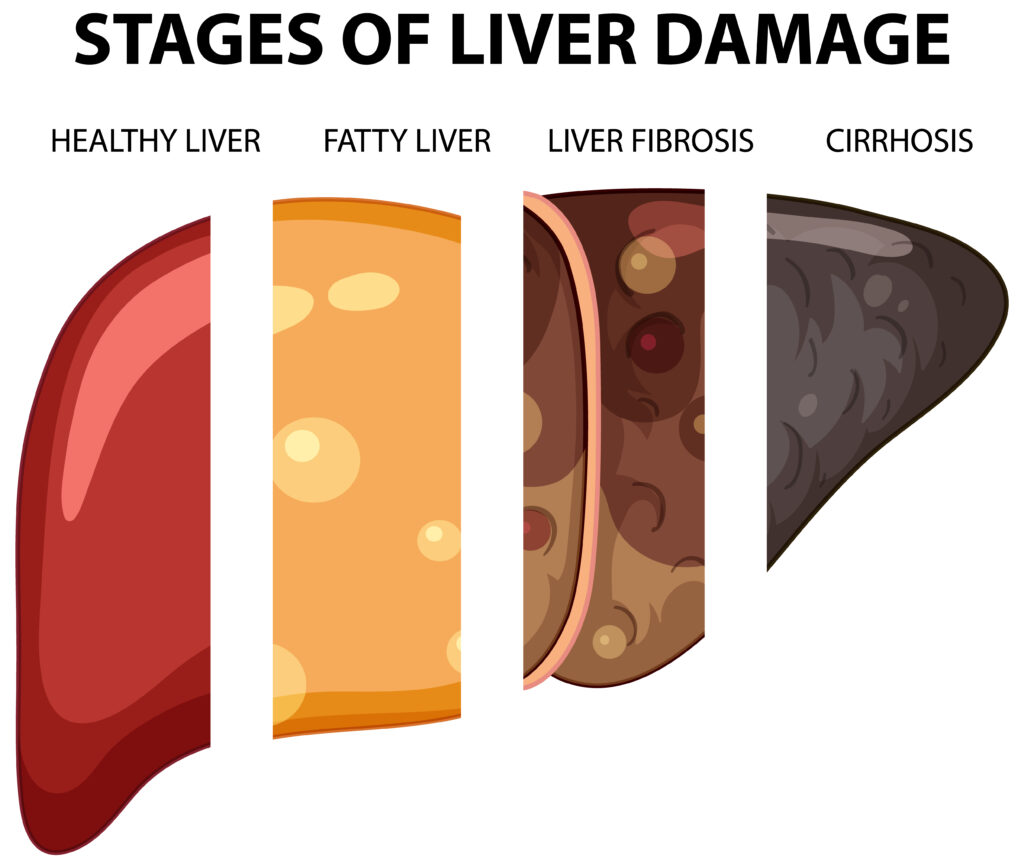
Elevated liver enzymes often indicate inflammation or damage to liver cells. When liver cells are inflamed or injured, they release higher-than-normal amounts of specific chemicals, including liver enzymes, into the bloodstream. This elevation in liver enzymes can be identified through routine blood tests. Typically, the increase in liver enzyme levels is mild and temporary, and it often doesn’t suggest a chronic or severe liver issue. Elevated liver enzymes may suggest an impairment in the proper functioning of the liver. Common causes include conditions like fatty liver disease and cirrhosis. Effectively managing these conditions is essential for addressing high enzyme levels.
Signs and symptoms
If elevated liver enzymes are due to liver damage, you might experience symptoms such as:
- Jaundice (yellowing of your skin or eyes).
- Abdominal (stomach) pain.
- Loss of appetite.
- Itching.
- Dark urine (pee).
- Light-colored stools (poop).
- Fatigue (feeling tired).
- Nausea and vomiting.
These symptoms could indicate potential liver issues, and it’s essential to seek medical attention for proper evaluation and management.
Causes of elevated liver enzymes
Various illnesses and situations may contribute to elevated liver enzymes levels. Your healthcare provider identifies the underlying cause by examining your medications, assessing your symptoms, and, if necessary, conducting additional tests and procedures.
More prevalent reasons for heightened liver enzyme levels encompass:
- Nonalcoholic fatty liver disease
- Obesity
- Over-the-counter pain medications, especially acetaminophen (Tylenol, others)
- Autoimmune hepatitis (liver inflammation triggered by an autoimmune disorder)
- Alcoholic hepatitis (severe liver inflammation resulting from excessive alcohol consumption)
- Heart failure
- Certain prescription medications, including statin drugs used to manage cholesterol
- Drinking alcohol
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Celiac disease (small intestine damage caused by gluten)
- Hemochromatosis (excessive iron stored in your body)
- Liver cancer
- Cytomegalovirus (CMV) infection
- Epstein-Barr virus
Treatment for elevated liver enzymes
The approach to addressing elevated liver enzymes levels hinges on the underlying cause. In instances where nonalcoholic fatty liver disease or metabolic syndrome is suspected by your doctor, lifestyle adjustments become pivotal. This involves monitoring your diet, refraining from alcohol consumption, managing weight, and regulating cholesterol levels. For individuals with obesity or moderately elevated liver enzymes, fibrates and statins are deemed safe pharmaceutical options for hyperlipidemia treatment.
Natural ways to maintain liver enzymes

If you have non-alcoholic fatty liver disease (NAFLD), it’s essential to be mindful that not all diets and supplements are liver-friendly. Before attempting any alternative treatments, it’s crucial to consult with your doctor.
⦁ Shed Excess Weight: According to the American Association for the Study of Liver Diseases (AASLD), weight loss is pivotal in improving NAFLD progression and symptoms. Losing 3-5% of body weight for those with obesity and NAFLD can reduce liver fat, and a 7-10% loss can improve other symptoms.
⦁ Consider the Mediterranean Diet: Research suggests that the Mediterranean diet may reduce liver fat, even without weight loss. This diet, beneficial for NAFLD, emphasizes plant-based foods, healthy fats, legumes, fish, lean meats, and whole grains.
⦁ Embrace Coffee: Studies indicate that coffee stimulates liver enzymes, offering protective benefits. Regular coffee consumption is associated with reduced overall liver damage in people with NAFLD.
⦁ Stay Active: NAFLD is linked to a sedentary lifestyle, and inactivity contributes to associated conditions. Aim for at least 150 minutes of moderate-intensity exercise per week to promote liver health.
⦁ Avoid Added Sugars: Dietary sugars like fructose and sucrose are linked to NAFLD development. Limit intake of added sugars found in baked goods, candies, sugary drinks, and processed foods.
⦁ 6. Address High Cholesterol: NAFLD can make it challenging for the body to manage cholesterol. Manage cholesterol by limiting saturated and trans fats, incorporating lifestyle changes, and considering medication if prescribed by your doctor.
⦁ Try Omega-3 Supplements: Omega-3 fatty acids found in certain foods and supplements may reduce liver fat and improve cholesterol levels, benefiting those with NAFLD.
⦁ Avoid Liver Irritants: Substance such as alcohol, certain medications, and some vitamins can stress the liver. Even moderate alcohol consumption can contribute to disease progression in NAFLD.
⦁ Inquire About Vitamin E: Vitamin E, an antioxidant, may reduce inflammation caused by NAFLD. Consult with your doctor to determine if vitamin E supplementation is suitable for your condition.
⦁ Explore Herbal Remedies: Certain herbs and supplements, including turmeric, milk thistle, resveratrol, and green tea, have been explored for their potential positive effects on liver health. However, it’s essential to consult with your doctor before incorporating these into your routine.
Remember, personalized advice from your healthcare provider is crucial before making significant lifestyle or dietary changes.